Doctors
Institutions
Conditions
Drugs
Insurances
TCM
Research
About Us
Contact Us
What is aortic stenosis?
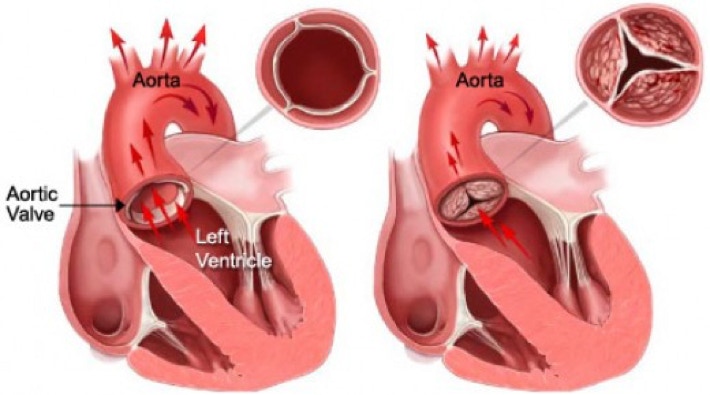
The aortic valve is one of the four valves inside the heart. It normally consists of three leaflets, or cusps, and separates the main pumping chamber of the heart and the aorta, the body’s largest artery. When oxygen-rich blood leaves the heart, it flows through this one-way valve, into the aorta.
In aortic stenosis, the aortic valve does not open fully and flow through the valve is restricted. The heart then has to work harder to supply enough blood to the body. As the aortic valve becomes more narrowed, this extra work eventually leads to symptoms, such as shortness of breath, lightheadedness or fainting, extreme fatigue, or chest pain, often during activity or exertion. Left untreated, the heart may enlarge and become weakened in time.
Aortic valve replacement can improve symptoms and prevent weakening of the heart.
What are the risk factors for aortic stenosis?
Aortic stenosis more commonly occurs if you:
Are age 65 or older
Are male
Have untreated high blood pressure
Have a malformed heart valve
Have a history of rheumatic heart disease
What causes aortic stenosis?
The most common cause of aortic stenosis is a build-up of calcium in the leaflets, or cusps, of the aortic valve. This build-up thickens or stiffens the valve and prevents the valve from opening fully.
This calcium build-up typically occurs with aging and is not related to calcium in the diet or calcium supplements. Some people are predisposed, or have a greater tendency, to develop this condition than others. High blood pressure, high cholesterol or kidney disease may speed up the process. You cannot prevent aortic stenosis with lifestyle changes.
The aortic valve normally has three leaflets, or cusps (known as a “trileaflet” aortic valve). But some people are born with an aortic valve that has only one (unicuspid) or two (bicuspid) leaflets. Since there is a greater tendency for calcium build-up on these types of malformed valves, being born with a unicuspid or bicuspid aortic valve increases the chance that one will develop aortic stenosis in his or her lifetime.
Rheumatic fever is a disease that may cause scarring of the aortic valve and lead to aortic stenosis. Rheumatic fever occurs infrequently in the United States and is a less common cause of aortic stenosis.
What are the symptoms for aortic stenosis?
People with aortic stenosis typically have no symptoms until late in course of the disease, when there is severe restriction of the aortic valve’s ability to open. Symptoms usually are first noticeable during physical activity or exertion. Common symptoms include:
Shortness of breath with activity
Chest pain or pressure
Lightheadedness or fainting
Extreme fatigue
If left untreated, aortic stenosis worsens over time and may result in congestive heart failure: fluid in the lungs, swelling of the legs and breathlessness even at rest.
How is aortic stenosis diagnosed?
Your doctor may first detect aortic stenosis when listening to your heart with a stethoscope during a physical examination. Your doctor hears an abnormal sound, known as a heart murmur. This murmur may occur before any symptoms.
A cardiologist, a heart specialist, may then perform the following tests:
Echocardiogram—an ultrasound of the heart that can detect and determine the severity of aortic stenosis. This noninvasive test uses high-frequency sound waves to observe the motion of the aortic valve and measure the speed of blood flowing through it.
Cardiac catherization—a diagnostic procedure in which a doctor inserts a catheter (a tiny, hollow tube) into an artery leading to the heart, injects contrast dye and then takes moving x-ray images of the heart and blood vessels. This test may be required if your aortic valve needs to be replaced or, in rare instances, when the diagnosis of aortic stenosis is uncertain.
High-resolution computed tomography (CT)—an alternative form of heart and blood vessel imaging. Only available at some medical centers, this noninvasive test is particularly appropriate for young people with a low likelihood of heart disease.
How is aortic stenosis treated?
When deciding on the best course of treatment, your doctor will consider your age, general health, medical history and severity of symptoms.
If you have mild or moderate aortic stenosis, you will need to visit your doctor regularly and have periodic echocardiograms to make sure your heart function is still strong. But you may not require treatment.
As the condition progresses, your doctor may recommend surgical procedures to replace the faulty valve. Possible surgical procedures are:
Open-heart valve replacement surgery—with one of two kinds of replacement valves:
Tissue valves—These valves have limited durability, but do not require you to take anticoagulant or blood-thinning medication
Mechanical valves—These valves may last for decades, but you must take blood-thinning medication for the rest of your lif
Open-heart valve replacement may sometimes be combined with a heart bypass operation.
Transcatheter aortic valve replacement—a newer treatment option offered to people with severe aortic stenosis who cannot have open-heart valve replacement surgery. This procedure involves threading a new aortic valve through an artery in the upper leg to the heart.
Balloon valvuloplasty—a procedure to provide some temporary relief of symptoms. A cardiologist who specializes in interventional procedures like these inserts a tiny, hollow tube called a catheter into an artery leading to the heart’s aortic valve opening. When the valve is reached, a balloon at the tip of the catheter is inflated to widen the opening. Then the balloon is deflated and the catheter removed.